What is Managed Care?

Amanda DeMarzo
Dec 28, 2020
10 minutes read
Managed care is a method of optimizing patient health using evidence-based healthcare strategies and resources. The purpose of managed care is to enhance the quality of healthcare for all patient populations. Managed care revolves around the collaboration of health insurance plans and healthcare providers.
Managed Care includes healthcare plans that are used to manage cost, utilization, and quality. This is done by providing care to members and contracting with health care providers and medical facilities. The overall goal of managed care plans is to reduce costs for members while improving the quality and outcomes of their care.
Why is Managed Care Important?
Managed care is a crucial part of our healthcare system today. Often the term “managed care” is used interchangeably with “insurance” but there is a specific definition to managed care that distinguishes it from other health care insurances. Managed care revolves around three main purposes: cost, utilization, and quality.
Historically, our healthcare system has been a fee-for-service model where the physicians are paid for every service they provide to their patients. This encouraged physicians to provide more care and services than needed. But this also drove the healthcare costs up and increased delivery of medically unnecessary services. Alongside that, services provided to patients in this payment model do not always lead to the best patient outcomes.

Managed care came out around the 1980s to tackle this dilemma of growing costs and unnecessary healthcare services. Since then, it is the primary model for our health insurance today.
As shown through the National Health Expenditure (NHE) data, total national health spending per capita has come down to match the annual growth rate of GDP per capita. This shows a more sustainable growth rate for both the economy at large and the subset of health expenditure.
When the national health spending exceeds that of the growth rate of the gross domestic product per year, the health share of the economy will continue to rise. The Centers for Medicare and Medicaid Services (CMS) projects an increase in health expenditures and health costs by 2028, increasing to $6.2 trillion compared to $3.8 trillion in 2019.
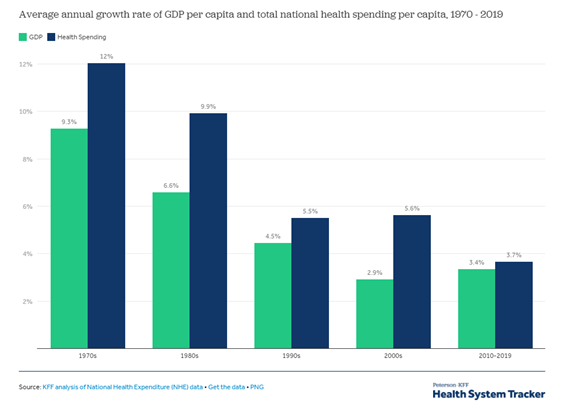
Figure 1: Average annual growth rate of GDP per capita and total national health spending per capita, 1970-2019. This provides insight into the growth of spending nationally in total and for healthcare. Too large of growth leads to unsustainable practices. Disproportionate health spending growth patterns show a faster spending growth in these areas. Learn More
The rate of growth for the healthcare spend can further be evaluated by the type of service provided (shown in Figure 2). The prescription medication average spend rate was much higher in the 1980s and 1990s. This puts a lot of pressure on health systems and patients to pay for prescription drugs and can be attributed to the increased number of drug approvals and booming pharmaceutical industry.
Since the introduction and implementation of managed care practices, we’ve seen the average spending rate for all healthcare services decrease and reach a more sustainable growth rate than the economy had previously experienced.
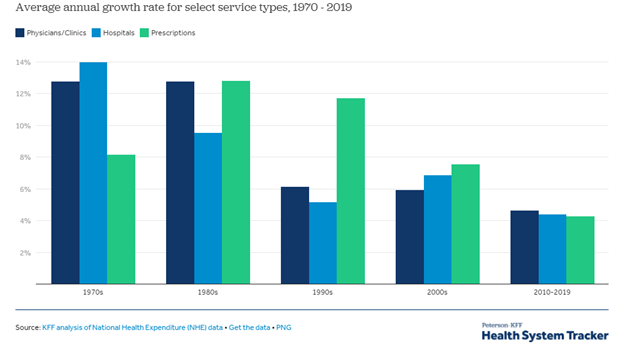
Figure 2: Average annual growth rate for select service types. The healthcare expenditure growth rate is evaluated by service type. Learn More
Managed care is a definitive move in our healthcare system to diverge away from fee-for-service and rather move towards value-based care. Ensuring a sustainable growth rate can help prevent the healthcare spend inflating faster than it already is.
Focusing on Patient Outcomes
In a value-based healthcare system, we focus on health outcomes and quality rather than the individual services provided. By evaluating the patient health outcomes, the providers are held to a minimum standard and if their services do not meet these standards, the providers do not get paid. This saves the entire health economy from paying for subpar health services.
This is further shown in the reimbursement model for episode-of-care payments, or bundled payments. An episode-of-care is the care a patient receives by a healthcare provider or health system for a specific illness, condition, or problem over a specific timeframe. A single payment is received for an episode-of-care. The provider is responsible for deficits that may raise the cost of the care provided. In some cases, this may include the cost of readmittance to a health facility for additional treatment for a length of time after discharge.
An example of an episode-of-care is pregnancy and delivery. In a fee-for-service model, care is paid in a piecewise fashion with little incentive to coordinate the care. In an episodes-of-care approach, the patient has inclusive care during pregnancy, delivery, after delivery for the mother, and after delivery for the baby. The incentive of great care during pregnancy is ensuring healthy birth weights for the baby upon delivery. This could prevent the baby from needing intensive care, costing an additional $100,000 on average.
Value-based-care promotes continuity of care and tries to bridge many different aspects of healthcare. This encourages a team-oriented approach to patient care. By implementing this model, we can ensure that the best quality services are provided to patients for a lower cost.
Types of Managed Care Plans
Managed care is a broad term that encompasses many types of insurance plans and organizations. The different types of managed care options differ in their cost and coverage of services. However, the common trait between these organizations is to keep costs low while still providing effective patient care.
Currently there are a few different types of managed care plan options that are available to patients, with the most notable ones being HMO, PPO, and POS. All valuing cost-effective patient care, these managed care plans vary in patient autonomy, coverage of services, and cost.
HMO, or Health Maintenance Organization, generally has a lower monthly premium payment compared to PPO and POS but requires the patient to designate a primary care provider within their network. All services utilized outside of the network are not covered by the HMO plan. When in need of a medical specialist, the patient must receive a referral from the primary care provider. By keeping the patient within the network, the managed care plan can guarantee a standard of care at a lower cost.
PPO, or Preferred Provider Organization, gives the patient more flexibility and autonomy in choosing where they want to receive healthcare services. PPO does not limit the patient to only their network but allows service outside the network, for a greater cost. The patients are not required to designate a primary care provider either and do not need referrals to see a specialist. With the increase in flexibility, however, monthly premiums tend to be higher than HMOs.
Finally, POS, or Point of Service, is the middle ground between HMO and PPO. POS generally has a higher monthly premium rate than HMO and requires a primary care provider to refer the patient to any specialist, but also allows healthcare services outside of the network for a higher copay.
What does managed care mean for health care professionals?
As mentioned previously, the aim of managed care is to improve quality of health care while also controlling costs. According to the Academy of Managed Care Pharmacy (AMCP), the goals of managed care include: disease prevention, enhancement of quality of life, increased clinical outcome benefits, improvement of quality and accessibility of care, and to ensure appropriate therapy for patients. To achieve these goals there is an emphasis on using standards for choosing providers and taking measures to improve care quality.
Providers are typically required to coordinate a variety of services for patients to ensure care is appropriate. Providers, typically primary care providers (PCPs), are gatekeepers to more expensive and specialized care. Referrals and prior authorization for specialists, laboratory services, diagnostics, radiology, etc. are a standard practice to reduce costs in the managed care system.
For providers, managed care adds additional administrative tasks to the medical practice and holds them accountable for practicing according to the most recent clinical guidelines.
What does managed care mean for patients?
The idea behind managed care has many benefits for patients. The main concept of improving quality and access while bringing down costs would be great for patients. This would ensure better health outcomes without increasing the national drug spend.
The intention of reducing costs and improving quality can be seen throughout the entire healthcare landscape. Despite the increased focus on Health Economic Outcomes Research (HEOR), increased quality metrics, and reviews of healthcare providers, we continue to see cost be the major concern.
Implementation of managed care has been primarily focused on cost reduction. We see more barriers to patient access as a widespread way to curb costs. These practices, like utilization management and prior authorization, can restrict patients access to necessary medicines and services. This hardly improves quality for better patient outcomes.
Restrictions to necessary medicines and services can be at a greater cost to the healthcare economy. With limitations to the type of care received, patients may not be able to see timely results. Patients are often required to navigate the healthcare systems as disease progresses. This leads to more expensive costs for treatments long-term.
How does managed care fit into the future of healthcare?
The current healthcare landscape is more sustainable than it had been previously, but the cost of healthcare continues to grow. CMS continues to express concern for a growing elderly population and the higher costs for supplying this population with healthcare.
For managed care to have a place in the future of healthcare, more focus will have to be directed on quality. Quality care in the present leads to higher cost savings long-term and that is the only way healthcare costs can be curbed.

Become excellent in prior authorization, reimbursement & market access: Become a prior authorization certified specialist
PACS Links
What is PACS?
PACS reviews
Why certify?
PACS price
PACS recertification
PACS extension
PACS FAQs
Quick contact
info@acmainfo.org